CAR-T Therapy: When the Immune System Becomes a Smart Weapon Against Cancer
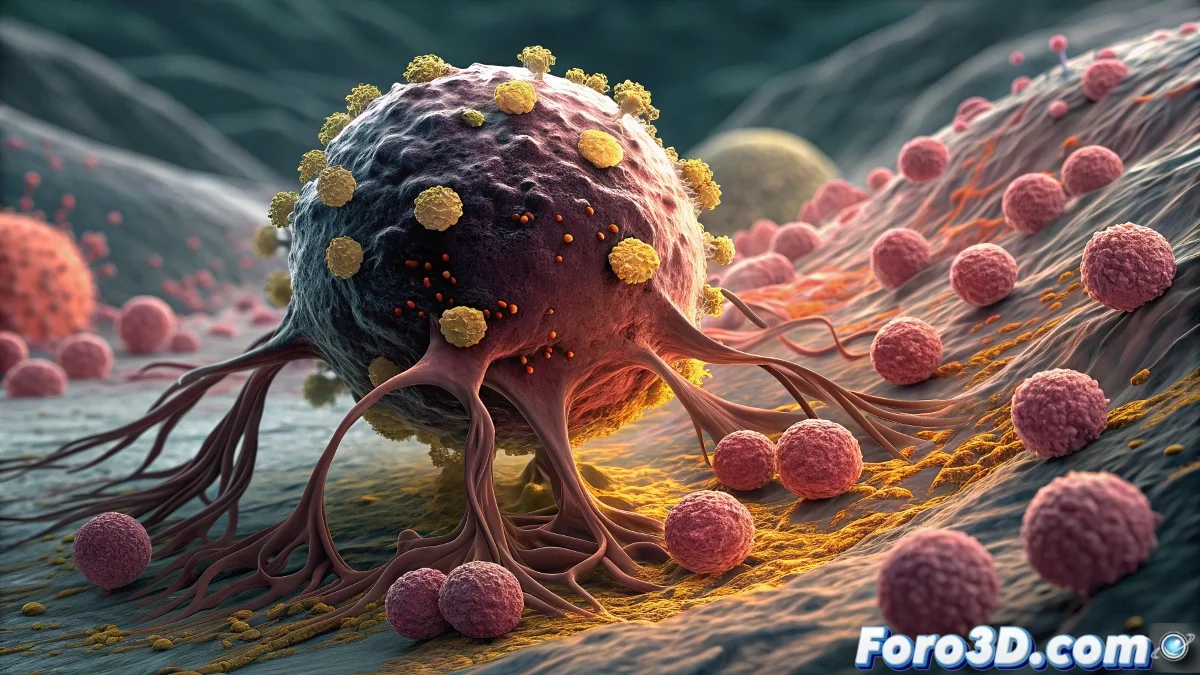
CAR-T therapy (Chimeric Antigen Receptor T-cell) represents the culmination of decades of research in cancer immunotherapy, offering a radically personalized approach against cancer. This cutting-edge technology transforms the patient's own immune cells into living drugs programmed to specifically recognize and destroy tumor cells. What began as a last-resort treatment for refractory leukemias and lymphomas is rapidly evolving toward broader applications, redefining what personalized treatment means in oncology. 🩸
The Process of Personalized Cell Engineering
The magic of CAR-T lies in its highly individualized manufacturing process. It all begins with leukapheresis, where T lymphocytes are extracted from the patient's blood. These cells travel to specialized facilities where they are genetically modified using viral vectors to express chimeric receptors that combine antibody recognition domains with T lymphocyte activation domains. The result is super lymphocytes capable of recognizing specific antigens on the surface of cancer cells, activating with greater potency, and persisting in the body as memory guards against relapses.
Mechanism of Action: Biological Precision
CAR-T cells represent a qualitative leap over conventional treatments because they combine the specificity of monoclonal antibodies with the cytotoxic potency and immunological memory of T lymphocytes. Their intelligent design solves two fundamental problems of the natural immune response against cancer: the failure to recognize tumor cells as a threat, and inhibition by signals from the tumor microenvironment.
Modular Design of CAR Receptors
CAR receptors are modular constructs that include: an extracellular recognition domain (usually scFv from monoclonal antibody), a spacer domain, a transmembrane domain, and one or more intracellular signaling domains. Second- and third-generation CAR-T cells incorporate multiple costimulatory domains (CD28, 4-1BB) that enhance activation, proliferation, and persistence of the cells. This precision engineering allows optimization of different aspects of the response according to the type of cancer and the patient's characteristics.
Components of the CAR receptor:- tumor antigen recognition domain
- optimized spacer region
- multiple costimulatory domains
- signaling activation domain
Clinical Expansion Beyond Hematological Diseases
While CAR-T has demonstrated spectacular efficacy in hematological cancers such as acute lymphoblastic leukemia and diffuse large B-cell lymphoma, the true holy grail is its application in solid tumors. Challenges include identifying tumor-specific antigens, overcoming the immunosuppressive tumor microenvironment barrier, and ensuring safety by avoiding toxicity in healthy tissues. Current approaches investigate CAR-T targeting multiple antigens, CAR-T with safety switches, and combinations with other immunotherapies.
CAR-T is not a drug that is administered, but a process that is lived: from extraction to reinfusion of transformed cells.
Clinical Achievements and Success Stories
The results in certain types of cancer have been extraordinary. In refractory acute lymphoblastic leukemia in children, anti-CD19 CAR-T has achieved complete remission rates above 80%, with many patients maintaining remission years after treatment. In diffuse large B-cell lymphoma, response rates exceed 50% even in patients who have exhausted all conventional options. These successes have led to the approval of multiple CAR-T products by regulatory agencies worldwide.
Approved indications:- refractory acute lymphoblastic leukemia
- diffuse large B-cell lymphoma
- mantle cell lymphoma
- advanced multiple myeloma
Challenges and Future Direction
Despite the enthusiasm, CAR-T faces significant challenges: cytokine release syndrome and neurotoxicity require specialized management; exorbitant costs (often exceeding 300,000 euros) limit access; and manufacturing time (3-4 weeks) can be prohibitive for patients with rapidly progressive disease. Research focuses on developing off-the-shelf CAR-T from universal donors, reducing toxicities through safety switches, and expanding applications to common solid tumors like lung, breast, and colon cancer. 🎯
Areas of active development:- allogeneic CAR-T (from donors)
- multi-antigen targeting
- combination with checkpoint inhibitors
- improvements in manufacturing process
In the end, CAR-T therapies represent the realization of the dream of personalized medicine: treatments specifically designed for each patient and their particular disease, although the path to universal accessibility remains long and complex. 🔬