3D Bioprinting of Custom Corneas: The Swiss Revolution Against Blindness
The global shortage of cornea donors affects millions of people at risk of blindness, a problem that traditional medicine has not been able to fully solve. Facing this challenge, Swiss scientists from the Federal Institute for Materials Research and Testing (Empa) are developing a revolutionary solution: personalized cornea implants using 3D bioprinting. This innovative technique allows for the creation of artificial corneas that perfectly adapt to the unique anatomy of each eye, using a special collagen and hyaluronic acid hydrogel that can incorporate the patient's own stem cells to regenerate damaged tissue. This advance promises not only to solve the critical donor shortage but also to significantly reduce post-surgical complications and immune rejections.
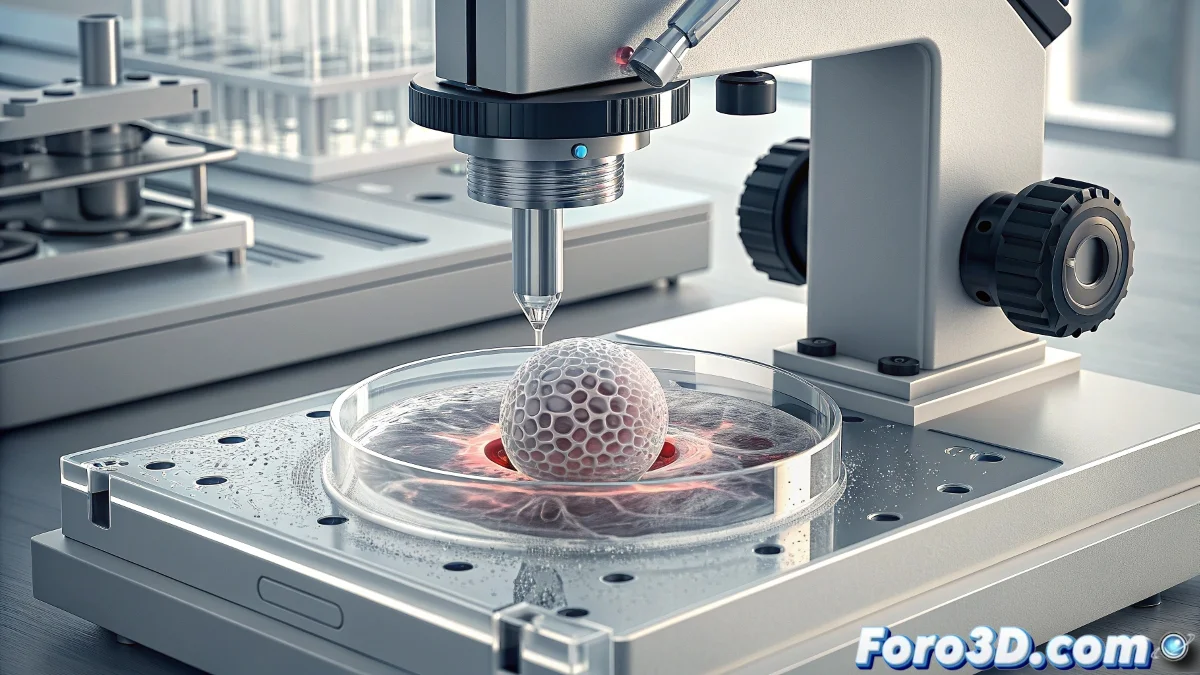
The Precision of 3D Bioprinting Applied to Ophthalmology
The process developed by Empa represents a qualitative leap in ocular tissue engineering. Unlike traditional methods that use standardized corneas, 3D bioprinting allows for the creation of implants that replicate with millimeter accuracy the specific curvature and thickness of each damaged cornea. Researchers use corneal topography data obtained through specialized scans to digitally design the perfect implant for each patient. This extreme personalization is crucial to ensure perfect integration with the remaining ocular tissue and optimize visual outcomes after the procedure.
Key Components of the Bioprinting Hydrogel:- Collagen as the main structural component
- Hyaluronic acid to promote hydration and biocompatibility
- Chemokines to guide cell growth
- Growth factors to stimulate tissue regeneration
- Biomarkers to monitor implant integration
Tissue Regeneration with Autologous Stem Cells
The true innovation of this approach lies in its ability to incorporate the patient's stem cells directly during the printing process. These cells, usually obtained from limbal tissue of the patient's healthy eye, are mixed with the hydrogel bio-ink before printing. Once implanted, the biological scaffold not only physically replaces the damaged cornea but also activates and guides the natural regeneration process. Over time, the stem cells proliferate and differentiate, progressively integrating the implant with the surrounding ocular tissue until a fully functional and biologically active cornea is formed.
This technology turns the patient into their own donor, eliminating the risk of immune rejection.
Overcoming the Limitations of Conventional Transplants
Traditional cornea transplants depend entirely on the availability of deceased donors and carry significant risks of immune rejection, infection, and surgical complications. Empa's approach addresses these problems comprehensively. As a biocompatible and personalized material, the hydrogel implant drastically reduces the immune response. Furthermore, the possibility of producing it on demand eliminates waiting lists and the preservation problems associated with donated tissues. The surgery is less invasive and the postoperative period is shorter with less immunosuppressive medication.
Advantages Over Conventional Transplants:- Immediate availability without dependence on donors
- Drastic reduction in the risk of immune rejection
- Anatomical personalization for better visual results
- Less invasive surgical procedure
- Faster recovery with fewer complications
- Possibility of treating complex conditions previously considered inoperable
The Path to Clinical Application
Although the technology is still in the preclinical research and development phase, the initial results are extraordinarily promising. In vitro trials have demonstrated excellent cell viability and proliferation on the hydrogel scaffolds, while tests in animal models have confirmed satisfactory integration with the host ocular tissue. The Empa team is now working on optimizing the optical properties of the material and validating the long-term stability